Case studies in diabetes management

By Anne N. Connor, director of community grants
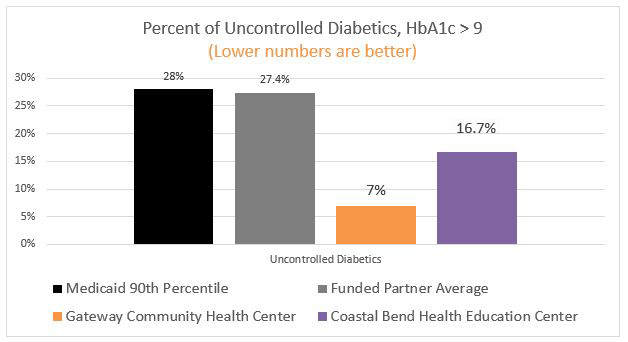
In 2015, two Methodist Healthcare Ministries funded partners, the Gateway Community Health Center in Laredo and the Texas A&M Health Science Center - Coastal Bend Health Education Center, did remarkably well at controlling HbA1c levels in diabetic patients.
The term HbA1c refers to glycated haemoglobin. It develops when haemoglobin, a protein within red blood cells that carries oxygen throughout your body, joins with glucose in the blood, becoming 'glycated.' By measuring glycated haemoglobin (HbA1c), clinicians are able to get an overall picture of what our average blood sugar levels have been over a period of weeks/months. For people with diabetes, this is important, since the higher the HbA1c the greater the risk of developing diabetes-related complications.
Both partners did well at controlling HbA1c in their adult diabetic patients. The rate of uncontrolled HbA1c in Gateway patients was 7%, and the Coastal Bend Health Education Center had a rate of 16.7 %, both better than the Medicaid 90th percentile.
When asked what made them successful, both organizations attributed it to the following components:
| Gateway Community Health Center: Leveraging long-term relationships | Coastal Bend Health Education: Consistency and support | |
| Integration | Diabetes programs were integrated into medical practice. | A multi-disciplinary diabetes education care team for diabetics included: a physician medical director, registered nurses, certified diabetes educator, registered dietitians and community health workers. |
| Supportive Intervention | Nutritional assessment and counseling: a 10-week diabetes self-management course included weekly outreach by phone to answer questions, and provided support and reminders. Bi-weekly support sessions provided group problem-solving and a buddy system. | A consistent patient-focused approach promoted lifestyle changes, diabetes self-management and social support. This included regular diabetes self-management education classes in English and Spanish, as well as monthly support groups and refresher trainings based on patient needs (i.e. glucometer training). Additionally, a three-part nutritional education course covered topics from food shopping to cooking to eating out. |
| Trusted Relationships | The community health workers that worked with patients and conducted the diabetes self-management courses had been with Gateway for over 10 years. This experience allowed staff to develop a rapport with patients and anticipate their needs. | Community health workers were integrated into the community and facilitated patient access to support services. They followed up on patient progress and made home visits when the patients were identified as high risk with cultural and linguistic barriers. Community health workers enhanced the quality and cultural competence of program service delivery by serving as advocates. |
| Clinical Knowledge | Careful, systematic monitoring of HbA1c at regular intervals helped move diabetics through different levels of support based on test results. | All diabetic patients received a follow-up appointment every three months that monitored the progress of their treatment plan. Biometrics were obtained (HbA1c, blood pressure, random blood glucose, weight, BMI and percent of body fat) so patients could see changes in their health. This monitoring also allowed patients with urgent needs (such as a very high HbA1c) to be referred to medical providers for one-on-one crisis care. |
| Patient Convenience | A one-stop shop model made it convenient for patients to access wrap-around services. Diabetic testing supplies were also provided year-round at low cost. | Diabetes self-management education classes were offered in the day and in the evening at convenient locations around the region. |